The Pinnacle Event for Behavioural Health, Addiction Treatment, and Mental Health Experts
Wednesday 26 April – Friday 28 April 2023
RACV Royal Pines Resort, Gold Coast
10 year high
Alcohol induced death rate is the highest in 10 years.
25% Increase
In 2020, around 2,600,000 Australians will have an addiction to drugs or alcohol. This number is up from 2,100,000 in 2017, an increase of 25%.
More Than 1%
The number of Australians who have a gambling problem doubled over 10 years, to more than 1 percent.
Over 70%
Over 70% of internet addicts also suffered from other addictions.
Statistics: aihw.gov.au, addictionhelp.com, washingtonpost.com
Designed for the sector, by the sector.
Create safer communities by reducing and managing substance use, addiction and harmful dependencies.
From alcohol and other drugs through to exercise, gaming, gambling, technology, food, and pornography, this three day conference encompasses all aspects of behavioural, mental, and chemical addiction.
We want to broaden and promote the understanding of substance use and dependency formation and explore the many ways in which we can put steps in place to prevent, treat, and support those in need.
United, our skills, practices, plans, and research findings can create better paths for prevention, treatment, and recovery.
“I can't recommend the Australian and New Zealand Addiction Conference highly enough. It is extremely professional, with knowledgeable presenters encouraging learning and networking in an ever-changing field of addiction.” – Susan, CatholicCare
Is this event for me
Yes! The Australian & New Zealand Addiction Conference is for you if you’re looking for:
| Application based presentations to leave you with practical tools to create immediate and positive changes for yourself, your clients and your community. | |
| Networking with like-minded AOD, behavioural and mental health professionals to discover best practice solutions. | |
| Inspiration from current research, top professionals and community leaders in the AOD and behavioural health sector. | |
| A platform to share your research, services, and case studies with the leaders in the AOD and behavioural health sector. | |
| A space to collaborate with and support likeminded professionals and services to deliver better outcomes for communities across Australia and New Zealand. | |
| A break away from your every-day to think bigger, creatively and strategically. |
Join us and walk away from the event connected, inspired and excited by your sector, it’s professionals and its future.
What our past delegates say
Keynote Speakers
Dr Gabor Maté
Bestselling Author and Internationally Renowned Speaker
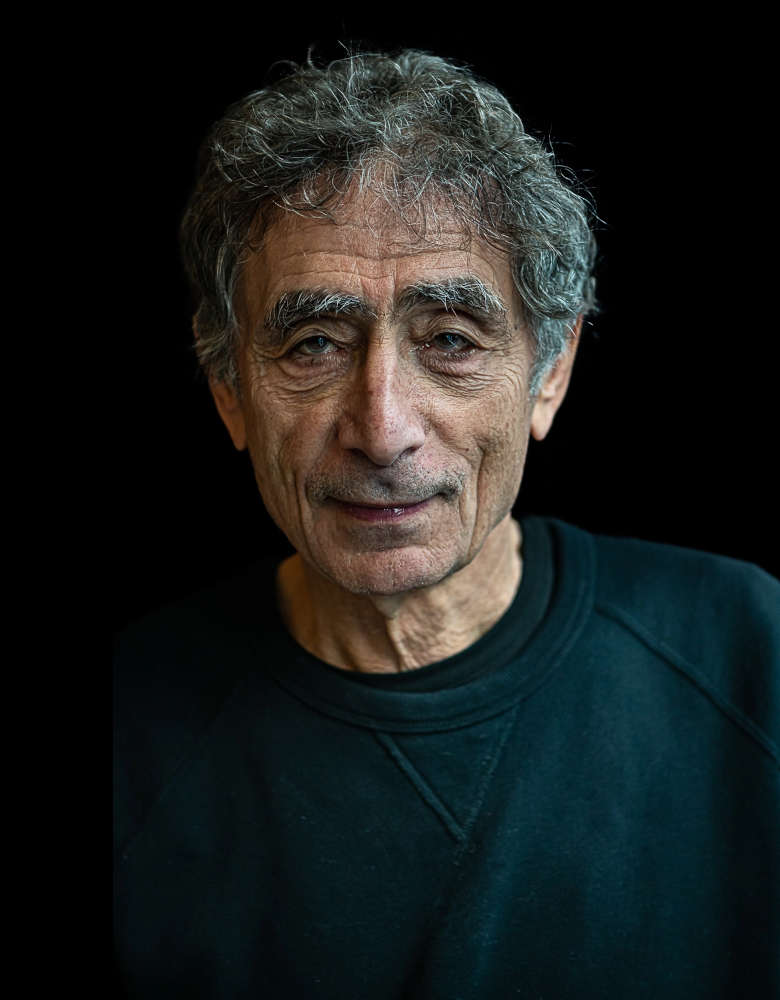
Dr Gabor Maté
Bestselling Author and Internationally Renowned SpeakerGabor Maté M.D., C.M., is a Canadian physician (retired), public speaker and bestselling author, published internationally in multiple languages. His book on addiction, the award-winning In the pg. 5 Realm of Hungry Ghosts: Close Encounters with Addiction, is used as a text in many institutions of higher learning in Canada and the U.S. His most recent book, The Myth of Normal: Trauma, Illness and Healing in a Toxic Culture, to be published in over 30 languages on five continents, has been and continues to be a #1 Canadian bestseller and, as of March 26, 2023, will been 18 weeks a New York Times bestseller.
After two decades as a family doctor and palliative care director, for twelve years Gabor worked in Vancouver’s Downtown Eastside with patients challenged by hard-core drug addiction, mental illness and HIV, including at Vancouver Supervised Injection Site, North America’s first such facility. His other interests encompass childhood developmental issues, ADHD, mind/body health, trauma and parenting. He is in constant demand as a speaker internationally and has addressed judicial bodies in Canada, the U.S. and Australia on the links between trauma, addictions, and dysfunctional behaviors. He has worked with many Indigenous communities around these issues.
He has received an Outstanding Alumnus Award from Simon Fraser University and an Honorary Degree (Laws) from the University of Northern British Columbia. For his groundbreaking medical work and writings, he has been given the Order of Canada, and the Civic Merit award from his home city of Vancouver.
A film based on his work, The Wisdom of Trauma, has been viewed by over 10 million people internationally and has been translated into twenty languages. It is shown regularly in many institutions, including schools and prisons, in Canada, the U.S., and abroad. www.thewisdomoftrauma.com. His therapeutic method, Compassionate Inquiry, has been, in the past three years, studied by over 3,000 health care providers in 80 countries. Gabor is a speaker much in demand internationally on addiction, stress and mind/body health, child development, trauma, ADHD and other topics related to his five best-selling books. He has been featured on some of the most popular podcasts, such as Joe Rogan, Tim Ferris, Jay Shetty, and others.
His next book, co-written with his son Daniel, will be Hello Again: A Fresh Start for Adult Children and Their Parents, based on their popular workshop.
www.drgabormate.com
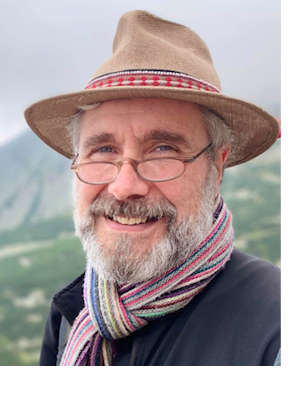
Edward Mantler
Mental Health Commission of Canada and Co-Chair, HSO Technical Committee TC011 Mental Health and Addictions

Edward Mantler
Mental Health Commission of Canada and Co-Chair, HSO Technical Committee TC011 Mental Health and AddictionsA highly motivated visionary and an expert at building partnerships, fostering stakeholder engagement, and aligning strategic objectives, Ed has led innovation and improvement in both health care and mental health for over two decades.
As Vice-President of Programs and Priorities at the Mental Health Commission of Canada, Ed is dedicated to promoting mental health in Canada and changing the attitudes of Canadians toward mental health problems and illnesses. By collaborating with stakeholders to improve access to effective, high-quality mental health services and supports, he leads the way to change, nationally and internationally. Ed also directs efforts to advance the Mental Health Strategy for Canada, with attention to reducing stigmas and increasing mental resiliency through innovative measures like Mental Health First Aid, The Working Mind/The Inquiring Mind, workplace mental health, student mental health, suicide prevention, and research into the impacts of cannabis on the mental health of Canadians.
Ed is accustomed to wearing many different hats. As a Surveyor with Accreditation Canada, he contributes to quality and safety in health care across Canada and internationally. Ed is a Registered Psychiatric Nurse, holds a Master of Science Administration degree, and is a Certified Health Executive.
Judy Atkinson
Professor of Indigenous Australian Studies

Judy Atkinson
Professor of Indigenous Australian StudiesOf Jiman, Bundjalung, German and English ancestry, Judy Atkinson commenced a PhD after working in Queensland for the Aboriginal Coordinating Council, where she was confronted by the tragedy of colonial rule on her country men and women. She titled the outcomes of her PhD: Trauma Trails – Recreating Song Lines the transgenerational effects of trauma in Indigenous Australia. She continues to search for solutions, a way forward for all Australians, spending the last twenty years working both in the academy (as Professor of Indigenous Australian Studies) and Aboriginal communities across Australia, confronting the tragedies of the past and a possible way forward, for all our children.
Kaye Phillips
Ph.D. Executive Director, Global Programs, Health Standards Organization Canada

Kaye Phillips
Ph.D. Executive Director, Global Programs, Health Standards Organization CanadaA collaborative leader at heart, Kaye has been dedicated to partnering for people-centered quality healthcare services innovation and improvement for over 15 years.
As Executive Director, Global Programs at the Health Standards Organization (HSO), Kaye and her team lead and foster the experience and expertise of people, families, health professionals, specialists and policymakers from across Canada and around the world - to develop evidence-based standards, assessments and quality improvement tools to achieve safer, equitable, and higher quality care, locally and globally.
Kaye directs partnered initiatives that focus on quality mental health and addictions care and services for people and the workforce across the continuum of care, including the establishment of the new national Mental Health and Addictions standard and Suicide Prevention Program standard and Canada’s Improving Integrated Care for Child and Youth Mental Health collaborative.
Promoting mental health services integration, psychological health and safety and trauma informed care practices, transcends across her teams work through partnered initiatives such as the British Columbia Cultural Safety and Humility standard the new national standard for Long-Term Care Services and the forthcoming national standards on Corrections Services in Canada, Pediatric Pain Management, Cannabis Use for Medical Purposes: Inpatient Care Settings, and Integrated People-Centred Spinal Cord Injury Rehabilitation standard.
As a family care partner, Kaye holds her lifelong personal experience navigating Canada's mental health and addictions services close to heart. With a deep dedication and love for her family and the outdoors Kaye is humbled on the daily in her personal and professional journey-to embrace the values, tips and tricks of mindful presence and leadership.
Kaye holds a PhD from the University of Toronto's School of Social and Administrative Pharmacy and serves on Canada's national Mental Health and Substance Use Advisory Committee.
Neavin Broughton
Board Member of the New Zealand Problem Gambling Foundation

Neavin Broughton
Board Member of the New Zealand Problem Gambling FoundationBio coming soon.
Tony Clarkson
Principal Clinical Advisor, Victorian Responsible Gambling Foundation

Tony Clarkson
Principal Clinical Advisor, Victorian Responsible Gambling FoundationTony trained as a psychodynamic psychotherapist for six years in London. He is the Vice-President of PACFA (Psychotherapy & Counselling Federation of Australia) and a board member with the South Eastern Melbourne Primary Health Network, where he also chairs the Clinical & Community Council.
Tony also co-chairs the National Mental Health Commission’s Self Stigma Technical Advisory Group, which contributes to the development of a National Stigma & Discrimination Reduction Strategy.
He currently works as the Principal Clinical Advisor at the Victorian Responsible Gambling Foundation (Victorian Department of Justice & Community Safety), where he provides clinical advice for a state-wide gambling addiction service system.
He was previously Clinical Manager at Connect Health & Community and Executive Manager of Psychological Services at Better Place Australia. Tony continues to work in private practice as a psychotherapist with long term patients who present with trauma, addiction and relationship issues.
Ashley Gordon

Ashley Gordon
Ashley is an Aboriginal Australian from the western-NSW community of Brewarrina, a descendent of the Gamilaroi and Barkindji people.
After a successful career in rugby league with the Newcastle Knights, Ashley is actively involved in the Gambling Help sector with extensive experience working with more the 200 Aboriginal communities throughout Australia. Ashley has vast experience in community education, awareness, help seeking and the delivery of successful programs for Indigenous peoples and communities.
Addressing the impacts of gambling in Aboriginal communities is his passion highlighted by the appointment to the federal Ministerial Expert Advisory Group on Gambling and the Expert Advisory Group for the Australian Gambling Research centre. A gambling counsellor with 20 years’ experience and six years has a gambling researcher with the Centre for Gambling Education and Research at Southern Cross University at Lismore. He currently joined the National Suicide Prevention Trial Evaluation Aboriginal and Torres Strait Islander Sub-Committee.
He is the Executive Director of NSW Aboriginal Safe Gambling Services, where he manages the GambleAware Aboriginal service, which targets Aboriginal communities and GambleAware organisations across NSW each year. He is also the First Nations Advisor for the Victorian Responsible Gambling Foundation. Ashley has a long-term objective to be involved in the ongoing development and implementation of Gambling related policies and programs that improve the well-being of Aboriginal people. Since the gambling question has been placed in the 715 Health Checks, Ashley been focusing on training to Aboriginal Health Workers.
Dr Nikola Ognyenovit
Dr Nikola Ognyenovit
Dr Nikola Ognyenovits is a Hungarian born Addiction Medicine Specialist Physician living in Brisbane, Australia. He has a strong interest in psychedelic science and its applications in substance use disorders, behavioural addictions and associated mental health conditions, including complex/developmental trauma, PTSD, depression, and anxiety disorders.
Currently he is working as a Staff Specialist in Metro North Alcohol and Drug Service in Brisbane and in private practice.
After training with The Ketamine Training Center in the US in 2018, he has incorporated Ketamine Assisted Psychotherapy (KAP) into his private practice in Brisbane. Dr Ognyenovits completed training with the Multidisciplinary Association of Psychedelic Studies (MAPS) in MDMA Assisted Psychotherapy to be a research therapist in a Monash/MAPS PTSD trial. As a Senior Lecturer in the School of Medicine at the University of Queensland he participates in medical education.
Dr Stuart Saker
Psychiatrist Toronto Private Hospital

Dr Stuart Saker
Psychiatrist Toronto Private HospitalBio coming soon.
Become a Presenter
Apply to present in 2023 and share your latest projects, programs, plans, and insights in treatment, prevention, and recovery with fellow sector professionals.
Over three days, we will explore the topics of:
THEME: Connecting, Collaborating and Creating Better Communities
- Harnessing technology & new treatment tools and protocols to pave the way forward in treating addiction
- Identifying development areas in prevention, treatment and after care services
- Revaluating treatment models and working towards true multidisciplinary care - what are some examples of this?
- Decriminalisation of illicit drugs - what does that mean for Australia and NZ?
- Changing the conversation - how do we change the stigma and judgement around addiction?
- Therapeutic potentials of Ketamine and other psychedelic medicines
- Understanding the influence of technology in behavioural addictions. What are the signs of technology addiction? Causes and how to prevent and stop.
Mental health and the rise of technology addiction in young children - trends and changes
Teens and technology - how can parents protect their teenagers from the dark side of the web? - Social media's effects on self-esteem and mental health
- The role of technology and access to addictive substances and behaviours
- Connected versus disconnected - social media has allowed us to connect with people from all over the globe, but are we more disconnected from ourselves than ever before? What impact has COVID had on our sense of connection, merging personal with professional?
- What are clinicians saying about telehealth?
- Exploring dual diagnosis between mental health and addiction/AOD. Best ways to integrate treatment models to provide effective treatment solutions?
- Bridging the gap - effective treatment models and services for vulnerable communities (rural, remote, Indigenous, LGBTQIA+ etc..)
- Upskilling the workforce on co-morbidity challenges
- Aftercare innovations - could services combine to provide effective after care services?
- Service integration - examples of related services working closely together
- What is the addiction workforce? Who can work with addiction?
- Connecting with communities to demystify addictions treatment and drawing on community resilience and wisdom in responding to addictions treatment needs.
- How best to support the workforce and it's development?
- What is the peer support role within addiction? How important is it, that peer support is included, supported and encouraged within the sector?
- How does cultural safety, or lack of, impact addiction service delivery for First Nations communities?
- Successful Māori, Aboriginal, Torres Strait Islander models of treatment and healing
- What do we need to do differently to better support indigenous communities?
Partner With Us
Explore partnership options and gain exposure for your organisation.
Partner with the Addiction conference and expand your company’s exposure to Australian, New Zealand AOD, behavioural health and mental health professionals. Showcase (and show off) the programs, services and initiatives which can help make all AOD, behavioural health and mental health professionals lives safer, easier and more supported. Our team can assist in creating custom partnership packages designed for your specific goals, so reach out today.
Sponsors
Accommodation
Run of House Rooms
Room only - $240 per night
Room + breakfast for one - $270 per night
Room + breakfast for two - $300 per night
Spa Suites
Room only - $340 per night
Room + breakfast for one - $370 per night
Room + breakfast for two - $400 per night
* Spa suites available on request - please contact the conference secretariat to book.
Accommodation can be booked when you register.
If you have any questions, please contact us.
Networking Function
Date: Thursday 27 April 2023
Time: 5:00pm - 6:00pm
Cost: Included in your delegate registration. $77 for guests.
Catering: Drinks and canapes will be provided.
Registration Options
In-Person
3 DAY PROGRAM
$1,199 + GST
- All keynote presentations
- All concurrent presentations
- Discounted accommodation rates
- Access to interactive conference app
- 5 star conference catering package
- Access to exclusive networking functions
- Complete online access to audio and visual presentations for 30 days post-event
- Printed conference materials
- Over 10 hours towards CPD points
- Your personalised certificate of attendance
- Exposure for your organisation
- Plus, chances to win great prizes!
Please fill in your details below to begin your registration.
Virtual
2 DAY PROGRAM
$549 + GST
- Live streaming of all keynote presenters
- Live streaming of all sessions in the plenary room over two day conference period
- Virtual presentations
- Complete online access to audio and visual presentations for 30 days*
- Over 10 hours towards CPD points
- Your personalised certificate of attendance
*Day 1 not included.
*Access to all audio and visual presentations will be made available 5 business days after the conference has taken place, and will expire 30 days after access has been granted. Options to extend access will also be made available after 30 days.
Please fill in your details below to begin your registration.
In-Person Group of Four
3 DAY PROGRAM
$3,400 + GST
Price For Four (4) People Only
- All keynote presentations
- All concurrent presentations
- Discounted accommodation rates
- Access to interactive conference app
- 5 star conference catering package
- Access to exclusive networking functions
- Complete online access to audio and visual presentations for 30 days post-event
- Printed conference materials
- Over 10 hours towards CPD points
- Your personalised certificate of attendance
- Exposure for your organisation
- Plus, chances to win great prizes!
Please fill in your details below to begin your registration.


FAQ
The conference will be held on the sunny Gold Coast in Queensland. The venue is the RACV Royal Pines Resort and we do have special discounted conference accommodation rates available for you. You can access these rates and secure your accommodation at the same time you register for the event.
The conference is being held over 2.5 days with day one being a half day of masterclasses with a later start. It looks like this:
Day one: Wednesday, April 26th. Start time: 1:00pm. Wrap time: 4:30pm
Day two: Thursday, April 27th. Start time: 8:30am Wrap time: 5:15pm
Networking function: 5:15pm - 6:15pm.
Day three: Friday, April 28th. Start time: 9:00am Wrap time: 5:00pm
One of Australia's most important days of national remembrance, ANZAC Day is held on Tuesday, April 25th, the day before the conference starts.
There are a few options for you to arrange your travel to the Gold Coast. You can decide to make a long weekend trip to the Gold Coast and travel up on 21st, 22nd or 23rd of April. Enjoy the weekend, take part in our Gold Coast ANZAC Day services, then attend the conference the next day.
In the coming weeks we will send more information of Gold Coast destination experiences and local ANZAC Day remembrance services to make the most of your trip.
If you do not travel before or on ANZAC Day, we've ensured the program starts later with time to travel on the morning of Wednesday, 26th. The conference commences for a half day of masterclasses at 1:00pm. The conference venue (RACV Royal Pines Resort) is roughly a 55 minute drive from the Gold Coast airport.
Our 2023 theme is: Connecting, Collaborating and Creating Better Communities
Topics include:
- Progressive change - embracing and cultivating new ways of prevention, treatment and recovery
- Addicted to tech - understanding the connection: technology, addiction and mental health
- Collaborating for change - how can addiction services better work together to provide integrated, holistic and evidence based diagnosis, care, treatment and support?
- Listening, sharing and learning from Indigenous communities
The program agenda can be found here: Click here.
Absolutely! On the night of Thursday, April 27th you can enjoy a networking function and connect with your fellow delegates. This is scheduled for 5:15pm - 6:15pm.
It does. You will be given a personalised certificate of attendance, counting towards ten hours of CPD points.
- AOD sector workers and mental health professionals
- Addiction experts and NGOs
- Psychologists and psychiatrists
- Researchers, peer workers and lived experience
- Rehab facility workers and leaders
- Government representatives and policy makers
- Anyone connected to the AOD sector
- You will gain best practices, new ideas and real solutions with applicable takeaways to transport into your work and your community.
- You'll have a platform to use your voice and experience to influence policy change and give your feedback to the decision makers.
- You'll be involved in multi-sectoral collaboration and use the conference to share knowledge, case studies and research in order to advance the prevention, treatment and recovery of current and future generations.
- You'll be a part of the conversation to address key mental and emotional health challenges facing addiction and improve access to adequate support services
- Enjoy networking opportunities and professional development at the same time in a different, inspiring environment.
- You'll gain access to the latest research, projects, programs and strategies to help meet the diverse and complex needs of your clients.





.png?width=150&height=150&name=Currumbin%20Clinic_Circle%20Logo_Orange%20(002).png)

.png?width=250&height=79&name=Star%20College%20Australia-RTO-WOP%20(1).png)





